Signs of Mental Illness: What to Watch For and When to Get Help
Most of us know someone who has faced hard days or felt lost in their thoughts. What we don’t often see are the early signs that something deeper could be wrong. Mental illness can show up in any family, at any time.
Recognizing the first signs matters because it can help people get support sooner. Early care can make the path to healing smoother. Spotting the changes in how someone thinks, feels, or acts gives loved ones a better chance to help. Knowing what to watch for can change lives, including our own.
Emotional Changes: Not Just a Bad Day
Life is full of ups and downs, but mental illness often creates changes that don’t just go away after a weekend or a good night’s sleep. We all have days when we feel off, but sometimes, emotions become stuck. These stuck feelings can be signs of something deeper, something that needs our attention. Being able to spot emotional changes early can help us step in and support someone before things get worse.
Persistent Sadness or Low Mood

Photo by cottonbro studio
Ongoing sadness isn’t just a passing mood or disappointment. When someone loses interest in things they used to enjoy, pulls away from friends or family, or seems empty even during happy times, these aren’t just signs of a bad day. This kind of sadness can last for weeks or months.
Common signs of persistent sadness include:
- No longer caring about hobbies or favorite activities
- Withdrawing from social contact
- Seeming tired or lost, even at special events
- Expressing feelings of worthlessness or hopelessness
It’s not always easy to spot, especially if someone tries to hide it. But when the joy is gone and emptiness takes its place, it’s time to pay attention. Learn more about the warning signs of chronic sadness and persistent depressive disorder symptoms.
Outbursts, Anger, and Irritability
Emotions can sometimes boil over. When someone gets angry over small things, snaps at loved ones, or struggles to keep their cool, it’s easy to chalk it up to stress. But frequent outbursts or a constant low simmer of frustration might signal more than just growing pains or work stress.
Possible warning signs:
- Explosive reactions to everyday problems
- Shouting or becoming mean over slight mishaps
- Feeling out of control during flashes of anger
- Quick mood shifts between calm and upset
Sudden anger and irritability often hide feelings like fear, pain, or sadness. Emotional overload can sneak into daily life, harming relationships and making it harder to enjoy simple moments. If any of this sounds familiar, you might find more answers in this helpful guide to symptoms of anger management issues.
Excessive Worry or Anxiety
Most of us worry now and then. But when worry fills every part of the day, it can feel like a storm that won’t let up. People with anxiety often struggle to quiet their minds. They might fidget, seem restless, or look lost in their thoughts.
Here are some signs anxiety is taking over:
- Trouble sleeping or relaxing
- Racing thoughts that keep looping
- Always expecting the worst, no matter how unlikely
- Feeling tense, even in safe or calm places
Anxiety isn’t always loud. Sometimes, it hides behind perfectionism, long to-do lists, or seeking a kind of safety that doesn’t exist. If worry starts making it hard to get through the day, you might want to look at these signs of generalized anxiety disorder.
Seeing these emotional changes in ourselves or others isn’t easy. Yet, they’re some of the most common ways mental illness shows up in everyday life. Recognizing them is the first step to reaching out or getting help.
Behavioral Shifts: When Actions Change
Our behavior is like a mirror, often showing what’s happening beneath the surface. Sometimes, changes creep in slowly, and other times they leap out overnight. When we see someone acting out of character—a once social person shrinking away, or a steady worker letting things slide—we need to pay attention. These changes often hold clues about mental illness. Here, we uncover the key ways our actions can shift when something is wrong inside.
Social Withdrawal and Isolation: Describe pulling away from friends, family, or usual activities.
A sudden need for more alone time isn’t the same as a quiet afternoon to recharge. Instead, social withdrawal becomes a pattern. People stop answering texts or calls. They skip birthday parties and family dinners. Even things they used to love—like watching movies with friends or playing sports—don’t spark their interest.
You might notice:
- Canceling plans without a real reason
- Staying home for long stretches, even when invited out
- Responding with short or dismissive answers
- Hiding away in their bedroom or office more often than before
Pulling away from social connections signals more than just being tired. According to the American Psychiatric Association’s warning signs, this kind of isolation can be a strong signal that help is needed.
Neglecting Responsibilities or Self-Care: Talk about declines in performance at work or school, and ignoring basic self-care.
Sometimes, mental illness steals our interest in daily routines. The once neat desk piles up with forgotten bills. Students who loved school start missing homework or skipping class. At work, mistakes add up. Chores and errands feel impossible.
Key signals of neglect include:
- Skipping showers, wearing dirty clothes, or not brushing teeth
- Letting dishes and laundry pile up for days or weeks
- Missing deadlines or skipping work without calling in
- Ignoring messages from teachers, bosses, or coworkers
Self-care goes out the window, making even basic grooming a struggle. For people who are usually organized, failing to meet their own standards is a major red flag. The Mayo Clinic’s mental illness symptom guide helps show how loss of interest in taking care of ourselves is often linked to deeper issues.

Photo by SHVETS production
Risk-Taking Behaviors: Explain sudden reckless actions, such as unsafe sex, substance abuse, or criminal behavior.
Not all signs of trouble come in the form of withdrawal or neglect. Sometimes, people act out. Sudden, risky choices pop up where careful decisions used to be. They may spend too much money, drive recklessly, or seek thrills with drugs, alcohol, or sex.
Watch for these changes:
- Breaking laws or shoplifting out of the blue
- Gambling large amounts of money
- Using drugs or alcohol in unsafe ways
- Having unprotected or impulsive sex
These behaviors often feel urgent or risky. People take big chances without thinking about the fallout. The Mayo Clinic’s symptoms and causes of mental illness and the advice from Psychiatry Fort Worth regarding risky behavior both point to impulsive actions as strong signals that professional support may be needed.
When we or someone we know shifts in these ways, it’s much more than a string of bad decisions. Often, it’s a silent call for help.
Physical and Cognitive Warning Signs
Not all clues of mental illness show up in how we act or feel. Many signs run deeper, showing themselves in our bodies or the way our mind works. Sometimes, these early whispers get dismissed or chalked up to stress, a busy week, or age. Yet, these physical and thinking difficulties can sound the alarm long before illness grows. By staying alert to these changes, we give ourselves and loved ones a better shot at early help.
Sleep and Appetite Changes
Sleep and hunger are the body’s rhythm keepers. When mental health starts to falter, these patterns often stumble.
- Trouble falling asleep, waking up through the night, or sleeping long past sunrise can all point to trouble.
- Some may feel exhausted but still can’t rest. Others end up in bed for hours longer than before.
Appetite tells a similar story. A sudden drop in hunger or constant cravings both matter.
- Skipping meals or losing interest in food can cause weight loss without trying.
- Eating much more than usual, even without hunger, can lead to quick weight gain.
Long-lasting changes signal more than “bad days.” The American Psychiatric Association’s list of warning signs highlights these shifts as common red flags of illness taking hold.
Physical Complaints Without Clear Cause
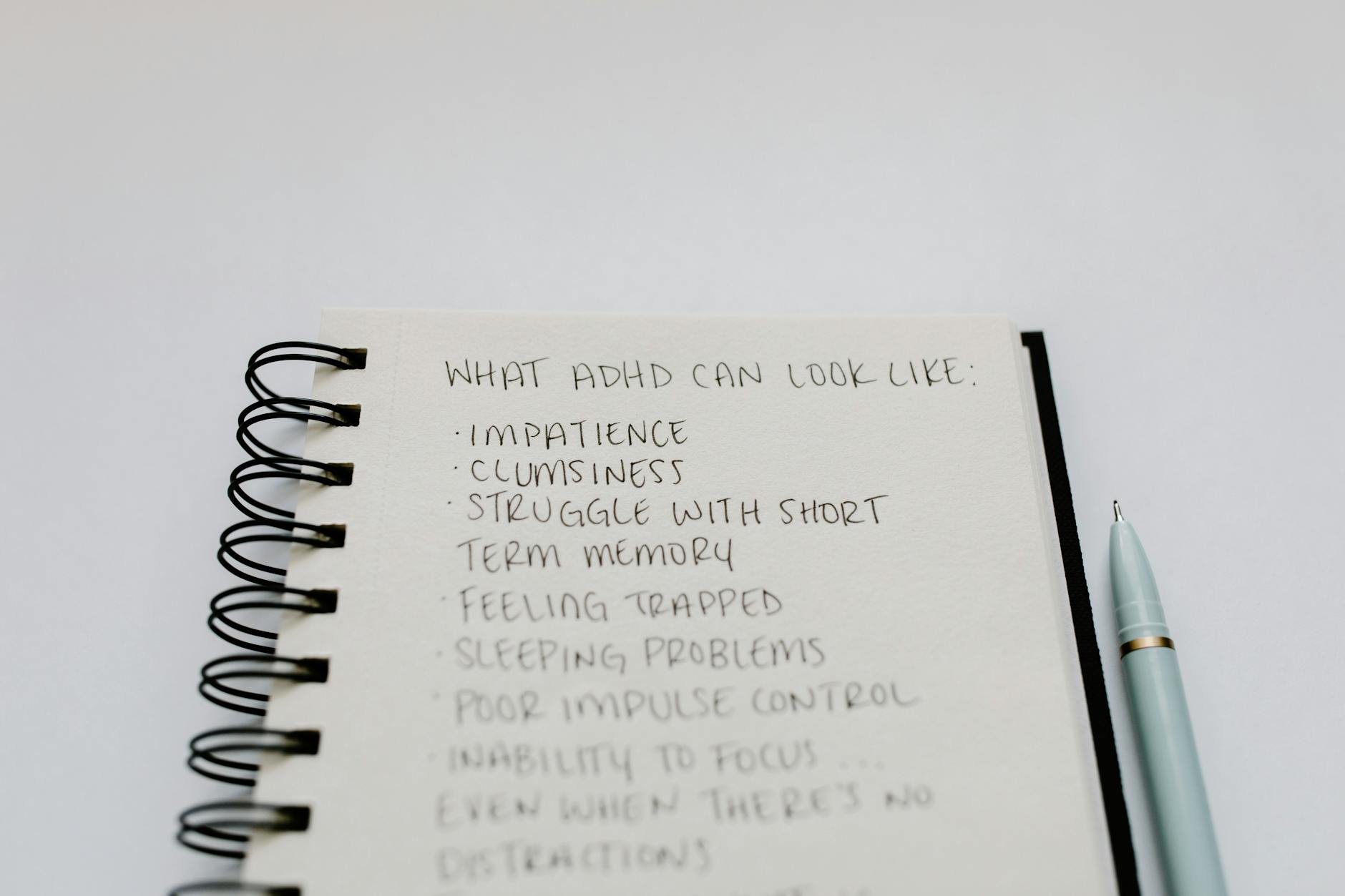 Photo by Tara Winstead
Photo by Tara Winstead
Our minds and bodies are linked. When the mind battles stress or sadness, the body often keeps the score.
Common complaints can include:
- Headaches that don’t fade with basic treatments
- Stomach aches or cramps without illness or food issues
- Aches, pains, or unusual soreness in joints or muscles
- Feeling tired all the time, even after rest
When a doctor finds no medical cause, these symptoms may come from mental strain. The Mayo Clinic lists these as possible first signs of mental illness—especially when they linger.
Difficulty Thinking or Concentrating
Mental illness isn’t just about mood. It can tug at how we think, remember, and focus.
Common signs we might see:
- Forgetting appointments or simple tasks
- Losing our train of thought mid-sentence
- Struggling to finish work or chores
- Trouble keeping up in conversation or at school
Tasks that felt easy may now require real effort. Some people describe it as “brain fog,” where thoughts move slow or get jumbled.
Minds that once zipped now crawl. These difficulties reach beyond absentminded moments and can signal that help is needed. NAMI’s warning signs guide outlines these problems as early red flags for families and friends.
Paying attention to these shifts gives us power. Bodies and brains signal in quiet ways when care is needed. When we notice changes in sleep, hunger, pain, or thinking, it’s not a weakness. It’s a smart step toward healing and hope.
Warning Flags: Substance Abuse, Self-Harm, and Suicidal Thoughts
Some of the most serious signs of mental illness unfold when people try to numb pain or escape inner turmoil. Using drugs, alcohol, or even self-injury often serves as a hidden alarm. If these actions surface, they demand quick attention and open conversation. We can watch out for these signs and support loved ones on the edge of crisis.
Using Alcohol or Drugs to Cope: How Substance Use Masks or Worsens Pain
Turning to alcohol or drugs feels, for some, like hitting a mute button on pain or anxious thoughts. It might start out as a way to relax or “take the edge off,” but it’s easy for this habit to spiral. The more often a person relies on substances, the harder it becomes to handle life without them. What began as a coping tool can feed a much bigger problem.
Patterns to watch for include:
- Drinking or using drugs to forget stress, sadness, or fear
- Using substances alone or in secret
- Needing more to get the same relief
- Losing interest in once-loved activities because of substance use
- Trouble at work, school, or in relationships from drinking or drug use
Alcohol, marijuana, opioids, and other drugs can hide depression, anxiety, or trauma for a while. But substance use can also bring fresh pain: worse mood swings, withdrawal, shame, legal trouble, or accidental injury. As explained by experts at the Cleveland Clinic, substance use disorders can quickly become tangled up with mental health struggles. If it looks like a loved one is using substances just to feel “normal” or to face daily life, it’s time to reach out. Even a simple offer to listen might open the door to getting them help.
Looking for support or resources to start the conversation? The SAMHSA National Helpline offers confidential help, day or night.
Self-Harm and Suicidal Thoughts: Spotting and Supporting Someone in Crisis
Self-harm isn’t always obvious. Some people cut, burn, or hurt themselves in private, hiding scars under sleeves or bandages. Others talk about being a burden or disappear from friends and family for days. These are not cries for attention; they are calls for relief from pain that feels too hard to explain.
Key signs that someone might be self-harming or thinking of suicide:
- Wearing long sleeves or pants, even in hot weather, to cover scars
- New wounds or scars with shaky explanations
- Giving away prized belongings or saying goodbye
- Talking about feeling stuck, hopeless, or wishing life would end
- Increased risky or reckless behavior
 Photo by MART PRODUCTION
Photo by MART PRODUCTION
The pain behind self-injury or dark thoughts isn’t always visible, but the risks are real. Support means listening without judgment and never brushing off talk of harming oneself. We should take every mention of feeling trapped or not wanting to live seriously. As found in this medical overview on suicidal thoughts, even silent or nonverbal clues matter.
If we believe someone is thinking about self-harm or suicide, the safest step is to stay with them and get help right away. Trained support is available locally and online, offering guidance for those facing these challenges and for worried family or friends. The New Jersey Mental Health Cares resource can be a helpful lifeline.
Spotting these warning flags lets us step forward with care, compassion, and swift action. We don’t have to solve it all, but we do need to act — often, help is just one honest conversation away.
When and How to Seek Help
Noticing something feels wrong is brave. Acting on it can feel risky, but support is closer than it seems. There are safe ways to start talking, both with the people we trust and with professionals. Many of us worry about making things worse or saying the wrong thing. We might wonder if it’s “bad enough” to ask for help. But reaching out is one of the strongest things we can do. We break down what reaching out looks like—whether it’s with a loved one or with someone trained to help.
Talking With Loved Ones: Offer tips for honest, non-judgmental communication with someone you care about.
Opening up about mental health should feel safe. If we’re reaching out to support someone, or it’s time to share how we’re feeling, honest, open talk matters most. We don’t need perfect words. Care speaks louder than advice.
Some ways to make these talks honest and caring:
- Pick a quiet spot, free from distractions.
- Speak simply. Short and sincere is best.
- Listen more than we talk. Give space for silence.
- Avoid judging. Don’t rush to “fix” things right away.
- Stay open to all feelings—sadness, anger, even silence.
Showing attention matters. We can let them set the pace. If someone isn’t ready, we don’t need to push—they’ll know we care by our patience and steady presence.
For easy-to-follow advice and helpful tips, the SAMHSA guide on how to talk about mental health offers good steps for talking with friends and family.
Professional Support and Resources: List types of professionals, hotlines, and support systems available.
Sometimes the support we need goes beyond what loved ones can give. That’s where trained helpers come in. There are many ways to seek professional guidance, both in person and online.
Types of professionals and support options:
- Primary care provider: A doctor or nurse can help start the process and make referrals.
- Therapists and counselors: They listen, give advice, or teach skills to cope with stress, sadness, or anger.
- Psychiatrists: Medical doctors who can diagnose mental illnesses and prescribe medication.
- Social workers: They help find resources, support families, and can suggest further care.
- Peer support groups: People share their own experiences, offer comfort, and keep each other motivated.
Key resources and hotlines:
- SAMHSA National Helpline: Offers free help 24/7, call 1-800-662-HELP. Learn about SAMHSA and the help they offer
- National Institute of Mental Health: Directory of mental health resources and what to do next. Explore help for mental illnesses
- CDC’s mental health resource page: Lists crisis hotlines, support for families, and direct counseling lines. See CDC’s mental health resources

Photo by cottonbro studio
Support isn’t one-size-fits-all. Some of us want a formal setting, others feel better in a peer group or talking on the phone. The right help is the one that feels possible today.
Why Early Action Can Change Lives: Emphasize that acting early can help recovery, reduce stigma, and save lives.
Moving fast makes a real difference. Acting early means someone gets help before things spin out. It can soften the blows of illness and open more doors to healing. The earlier we reach for help, the less power shame or fear can have over us.
Why urgent action saves lives:
- It’s easier to treat symptoms before they become severe.
- Families can learn how to give better support.
- People stay connected to work, school, and life.
- Early support keeps hope alive, making recovery more likely.
- Taking action chips away at stigma. Sharing stories helps others open up too.
When help starts early, it’s like catching a small leak before the flood. Progress and healing feel out of reach when we wait too long, but acting now brings the best chance at a healthier tomorrow. Find out more about how quick support changes mental health for the better in this piece on the power of early intervention in mental health.
The best step is the one we take today—even if it’s a small one. Waiting holds us back. Reaching out can change the story for us and the people we love.
Conclusion
Spotting early changes in mood, habits, or health shapes how we care for each other. When we listen to these signals and reach out, we stop pain from spreading and open doors to honest talk. Openness breaks shame and shows we can always get support, even if hope feels far away. Thank you for reading and caring—with each step, we make it safer for everyone to share their story. If you notice changes in a loved one or yourself, speak up. Sometimes help begins with one small, honest word.


